In the realm of cardiovascular health, blood pressure plays a pivotal role, often dictating the overall well-being of an individual. One of the intriguing aspects of blood pressure regulation is the classification into dipper and non-dipper categories. This distinction sheds light on crucial physiological patterns that can significantly impact health outcomes. This comprehensive article aims to delve deep into the concepts of “Dipper vs Non-Dipper Blood Pressure” phenomena, exploring their significance, mechanisms, clinical implications, and management strategies.
What is Blood Pressure?
Before diving into the specifics of dipper and non-dipper patterns, it’s essential to grasp the fundamentals of blood pressure. Blood pressure refers to the force exerted by circulating blood against the walls of arteries as the heart pumps it through the body. It consists of two measurements:
- Systolic Pressure: The pressure in the arteries when the heart beats and pumps blood out.
- Diastolic Pressure: The pressure in the arteries when the heart rests between beats.
Measured in millimeters of mercury (mm Hg), blood pressure is typically expressed as systolic over diastolic (e.g., 120/80 mm Hg), with normal values being less than 120/80 mm Hg.
Understanding Dipper and Non-Dipper Phenomena
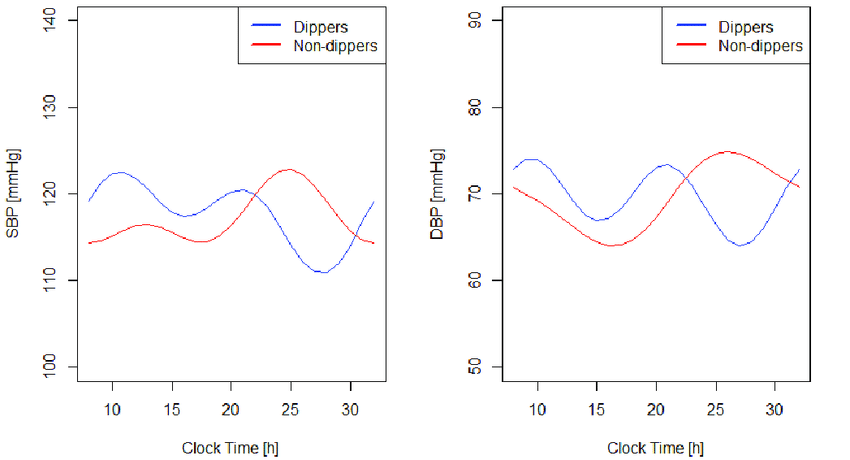
The terms “dipper” and “non-dipper” refer to patterns of blood pressure variation over a 24-hour period, particularly during sleep. These patterns are identified through ambulatory blood pressure monitoring (ABPM), which provides continuous readings over an extended period, offering insights into the circadian rhythm of blood pressure.
- Dippers: Individuals whose blood pressure decreases significantly (usually by 10-20%) during sleep compared to daytime levels are classified as dippers.
- Non-Dippers: Conversely, non-dippers are individuals whose blood pressure remains elevated during sleep, with minimal or no decrease compared to daytime levels (less than 10% reduction).
Mechanisms Behind Dipper and Non-Dipper Patterns
The mechanisms underlying Dipper vs Non-Dipper patterns are multifaceted and involve intricate interactions between the autonomic nervous system, hormonal factors, renal function, and circadian rhythms.
- Autonomic Nervous System: The autonomic nervous system regulates involuntary bodily functions, including blood pressure. During sleep, parasympathetic dominance typically leads to decreased sympathetic activity, resulting in lower blood pressure among dippers.
- Renal Function: Nocturnal changes in renal sodium excretion and water balance contribute significantly to blood pressure fluctuations. Dippers exhibit enhanced nocturnal natriuresis (sodium excretion), promoting blood pressure reduction during sleep.
- Hormonal Factors: Hormones such as renin, aldosterone, and cortisol exhibit diurnal variations, influencing blood pressure regulation. Disturbances in these hormonal rhythms can disrupt the dipper pattern.
Clinical Implications and Health Risks
Identifying whether an individual is a dipper or non-dipper holds clinical significance due to its implications for cardiovascular health:
- Cardiovascular Risk: Non-dippers have a higher risk of developing hypertension, left ventricular hypertrophy, coronary artery disease, stroke, and other cardiovascular complications compared to dippers.
- Target Organ Damage: Prolonged exposure to elevated nighttime blood pressure contributes to endothelial dysfunction, arterial stiffness, and target organ damage, accelerating cardiovascular disease progression.
- Therapeutic Considerations: Tailoring treatment strategies based on dipper status can optimize blood pressure control and reduce cardiovascular risk. Non-dippers may require more aggressive antihypertensive therapy or interventions targeting nighttime blood pressure.
Management Strategies
Managing dipper and non-dipper patterns involves a comprehensive approach aimed at promoting healthy blood pressure rhythms and minimizing cardiovascular risk:
- Lifestyle Modifications: Emphasizing regular physical activity, a balanced diet (low in sodium and saturated fats), weight management, stress reduction techniques, and smoking cessation can promote favorable blood pressure profiles.
- Pharmacological Interventions: Depending on individual profiles, antihypertensive medications may be prescribed to target specific blood pressure patterns and optimize control throughout the day and night.
- Monitoring and Follow-Up: Regular monitoring of blood pressure, particularly through ABPM, allows healthcare providers to assess treatment efficacy, adjust medications as needed, and mitigate cardiovascular risks associated with non-dipping patterns.
Conclusion
In conclusion, understanding the dipper and non-dipper phenomena provides valuable insights into blood pressure regulation and cardiovascular health. By recognizing these patterns and their implications, healthcare providers can tailor interventions to optimize blood pressure control, mitigate cardiovascular risks, and enhance overall health outcomes. Through continued research and clinical advancements, the management of dipper and non-dipper patterns continues to evolve, offering hope for improved cardiovascular health worldwide.